SUBOXONE VS VIVITROL VS SUBUTEX VS NARCAN VS…
Examining the differences between FDA approved medications to treat opioid use.
*Guest post by Aaron Haithcock
As what most insiders would consider a medium-well seasoned veteran of the rehab industry, I far too frequently come across misinformation and disinformation regarding the substances in the title. Unfortunately, training and education appears to be somewhat lacking at the top end, and the result is that the same small handful of misunderstandings get circulated ad nauseum within rehab and recovery communities.
My goal in writing this not-exactly-scientific document is to help those of us who rely on what is sometimes a concoction of get-better drugs, understand what exactly each substance does, both on its own, and in concert with others. My hope is that a clearer understanding of what is happening in our bodies when we take these drugs, will lead to a stronger ability for us recovering addicts to advocate for ourselves in the realm of medication-assisted treatment.
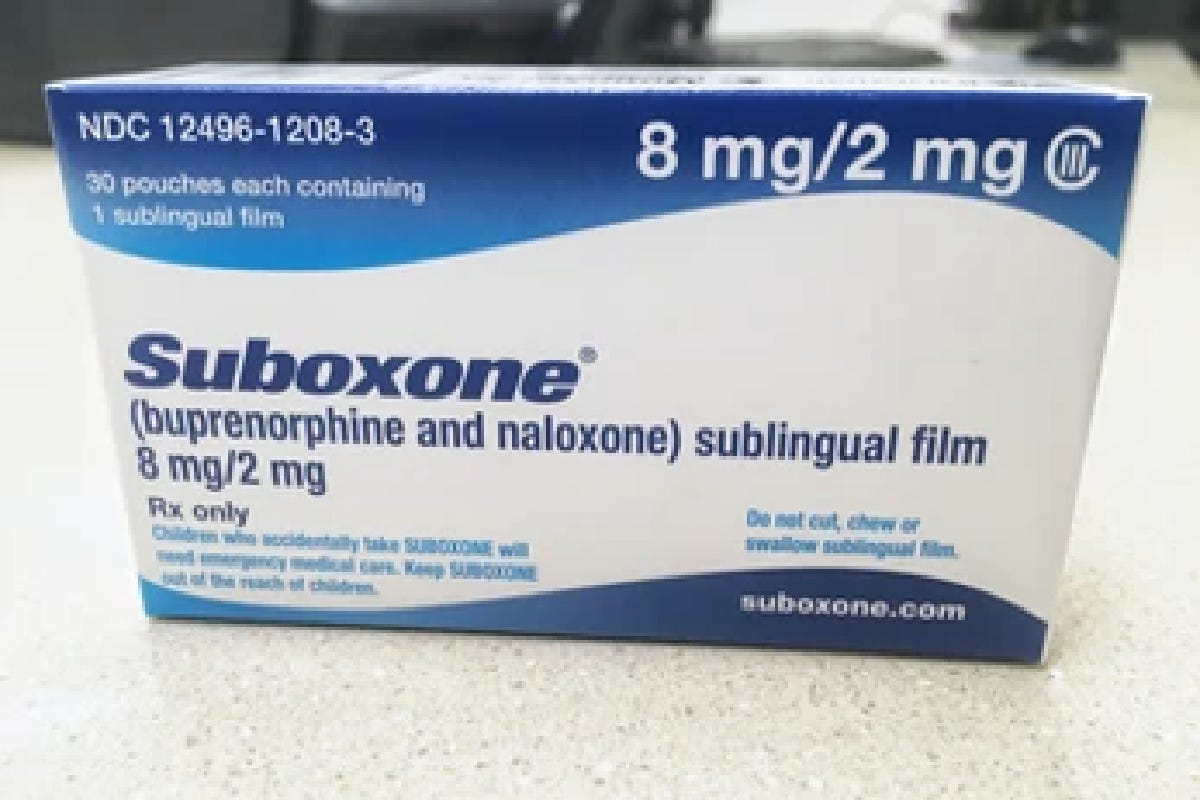
First I want to clear up some confusion by pairing each brand name I will discuss with its generic drug. Afterwards I will only refer to the drug by its generic name, not the brand name. Suboxone is a brand that contains buprenorphine and naloxone. Subutex is a brand that contains only buprenorphine. Narcan is a brand that contains only naloxone. Vivitrol is a brand that contains naltrexone, not to be confused with naloxone. I will therefore be discussing buprenorphine, naloxone, and naltrexone.
These three medications, plus methadone, are the only FDA approved drugs for helping with opioid dependence. They fall into two main categories: agonists, and antagonists. Buprenorphine is an agonist, meaning it interacts positively with opioid receptors in our brain. It stimulates them. Naloxone and naltrexone are both antagonists, meaning they attach to opioid receptors, but do not provide any stimulation. In fact, they bind so tightly that they prevent other substances from accessing the receptors they are attached to. So if a person does not have any opioid drugs active in their system, taking either naloxone or naltrexone will do nothing.
(Side note: naloxone and naltrexone are analogs of each other, meaning they are almost chemical identical, except for one small difference. This makes them chemical cousins. In this case, naloxone is a relatively short-acting antagonist, and naltrexone is its much longer acting cousin.Since naltrexone is so long acting, when given as a shot (Vivitrol) it will block almost all other opioids from binding to receptors, therefore preventing the ability to get high.)
The reason that you must wait a certain number of days until you may receive a naltrexone shot is because of its high affinity. Think of affinity as the level of magnetic attraction between any substance and its target; in this case naltrexone targeting opioid receptors. Naltrexone, naloxone and buprenorphine all have very high affinity (love for) our opioid receptors, much higher than other common opioids including fentanyl, and especially heroin. (Fun fact: heroin’s affinity for our opioid receptors is very weak, among the weakest of all the opioids. This does not mean that its potential to excite opioid receptors is weak). So if an opioid receptor is blissfully occupied by, say, heroin, and along comes either of the antagonists, naloxone or naltrexone, the antagonist will knock the weaker agonist off the receptor. Repeat this millions of times all over your body, and you are in precipitated withdrawal. (Since an opioid overdose doesn’t last nearly as long as a dose of naltrexone would, naloxone is used to reverse overdoses since it is so much shorter acting, about twenty-four hours for naltrexone, and one hour in the case of naloxone).
Now on to our agonist friend buprenorphine. The tricky thing about buprenorphine is that it is the only known partial opioid receptor agonist. Remember that it also has a very high affinity for our opioid receptors. This means that when buprenorphine binds to the receptor, it is only partially activated. That is why when you take a dose of Suboxone you may feel some euphoria (especially for those with little or no opioid tolerance), but your breathing and heart rate slows only a little. Constipation? Yes. Pinned pupils? Maybe. A full-blown opioid experience? Definitely not. But still, it is tightly bound to the receptor, and can only be knocked off by large doses of naloxone, which you wouldn’t need anyway.
What I hear so frequently is that if you take regular opioids when you’re on Suboxone or Vivitrol, you will get sick. This is not true. You will just be wasting your drugs and money, because none of the known full opioids can compete with the tight bond of buprenorphine or naltrexone. It is true, however, that if you take buprenorphine before you are starting to feel withdrawal symptoms, the buprenorphine will knock off your heroin/fentanyl or whatever, and you will be potentially very ill. And since buprenorphine lasts so long (about 36 hours) you will be sick for a long time. The only way to reverse that is to consume dangerous amounts of high-potent opioids, and even then, no promises.
In other words, it is the buprenorphine itself that precipitates withdrawal, not the naloxone or Narcan in Suboxone. If taken under the tongue, only about 30% of the buprenorphine and virtually none of the naloxone gets absorbed. Naloxone was added to the buprenorphine-only formula (aka Subutex) to deter people from injecting their buprenorphine. If you inject Suboxone, then the naloxone will knock off whatever opioids are on your receptors (including buprenorphine) but since naloxone is so short acting, the sickness would not last more than two hours tops.
I imagine that by now I have either thoroughly confused you or bored you. Maybe both. I’m no expert, but I speak from experience and hours upon hours of boredom-induced research. Feel free to do your own!
Thanks for reading,
Aaron Haithcock